What should you not do with spondylolisthesis
Contenuti
1# What is spondylolisthesis
2# What are the spinal symptoms caused by spondylolisthesis
3# What are the causes of spondylolisthesis
4# What are the complications of vertebral spondylolisthesis
5# How the diagnosis of spondylolisthesis is made
6# What treatments are adopted in spondylolisthesis syndrome and avoid the risk of paralysis
7# What to do and not to do with spondylolisthesis?
8# How to sleep with spondylolisthesis?
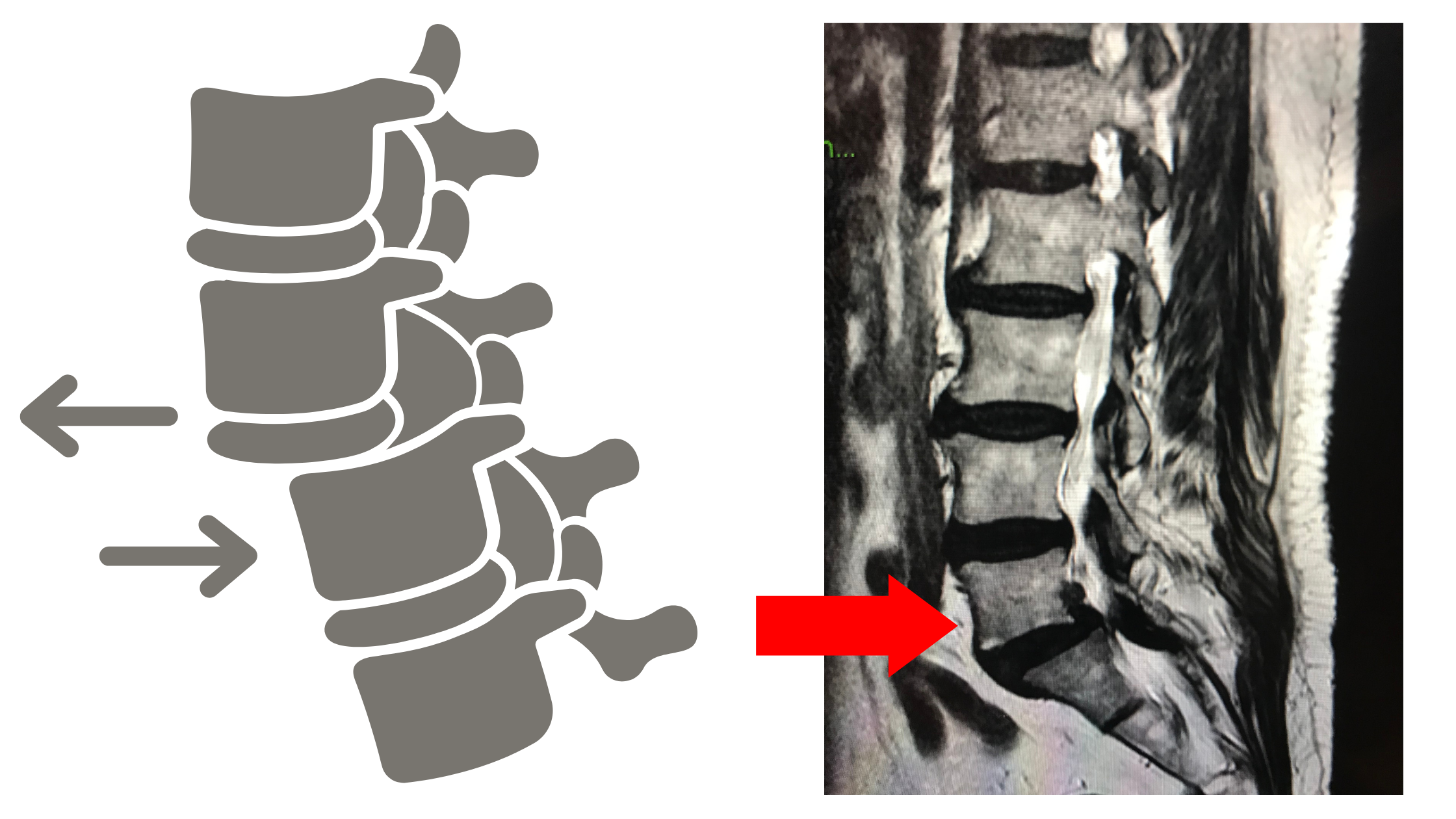
1# What is spondylolisthesis
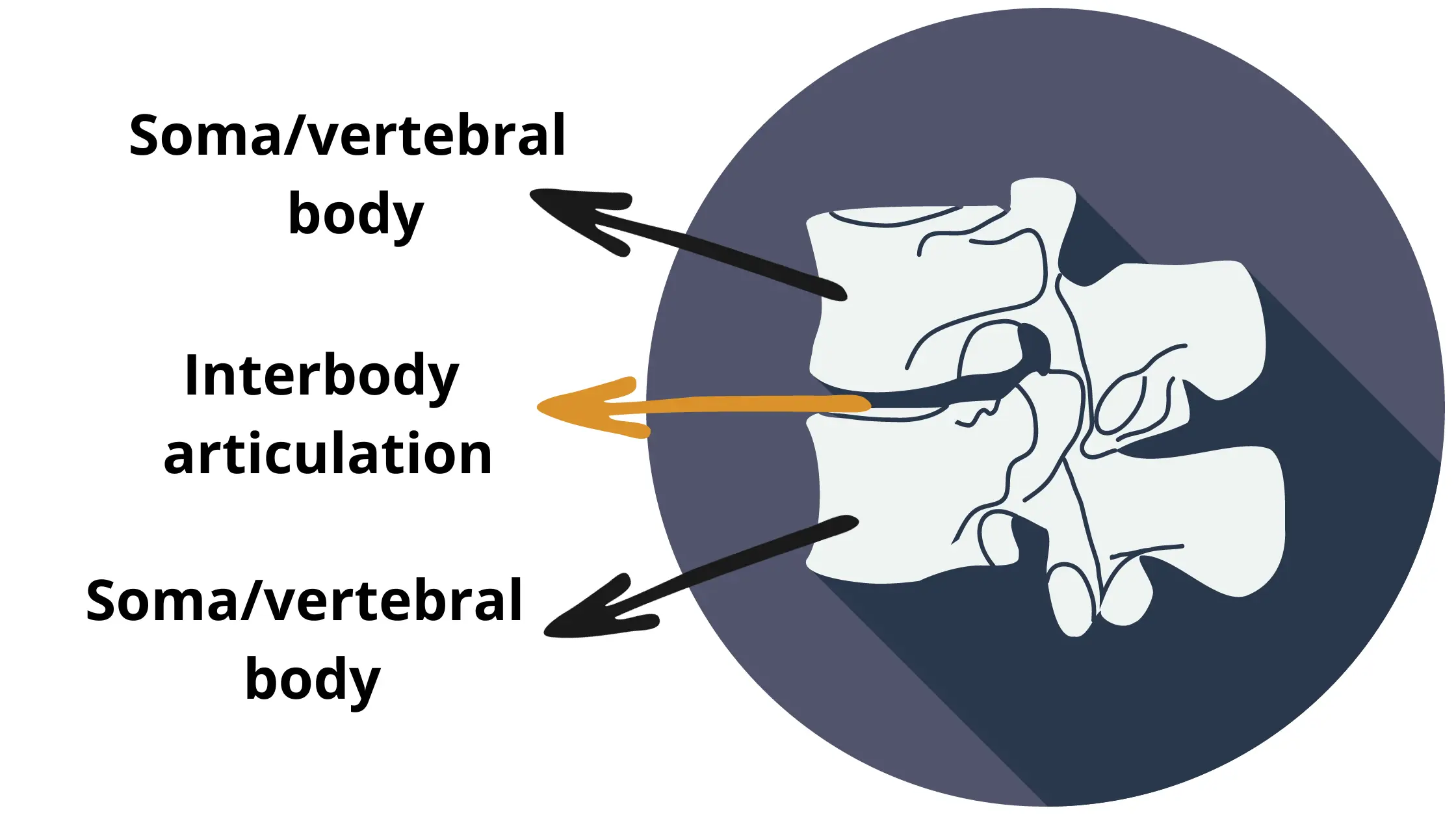
Spondylolisthesis is the sliding of a portion or all of the vertebral segment with respect to the underlying level.
There are three forms of vertebral slips:
Anterolisthesis: the upper vertebra slides anteriorly compared to the lower one;
Retrolisthesis: the upper vertebra slides posteriorly compared to the lower vertebra;
Lateral: lateral translation of the overlying vertebra.
It can affect different sections of the spine (for example it can occur at any level of the cervical spine), although the regions most affected are those between L4-L5 and L5-S1.
In normal conditions, the forward movement of a vertebral body is prevented mainly by the engagement of its articular processes with that of the underlying vertebra.
The insertions of the intervertebral disc and ligaments between the vertebrae also control this displacement, but to a lesser extent.

2# What are the spinal symptoms caused by spondylolisthesis
Spondylolisthesis is usually identified randomly during a radiographic examination following trauma, such as falls at home.
The first symptoms that may develop are low back pain that radiates behind or below the knee, with tightness in the hamstrings and difficulty bending forward with straight knees.
Leg lifting (like climbing stairs) is also very limited.
Standing tends to make symptoms worse.
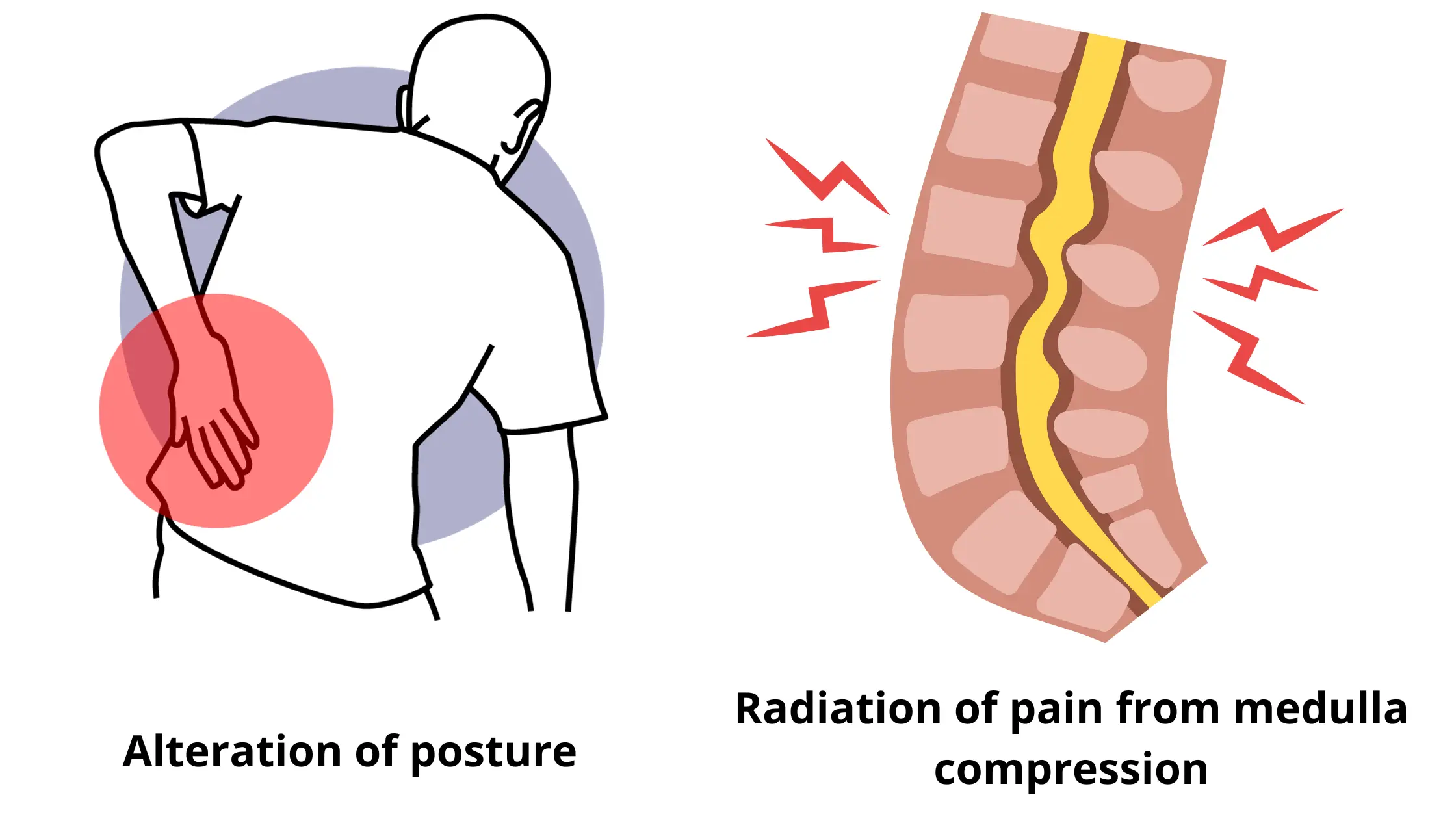
The clinical picture varies from the degree of slippage of the vertebra; an increase in it can lead to an alteration of posture, up to the most serious cases, which present severe and disabling symptoms.

Signs and symptoms present with:
- Pain, which increases with movement in all directions, in particular during extension of the back (in anterolisthesis) and with increased load (for example when carrying shopping bags);
- Radiation of pain to the buttock and the back of the thigh and leg (tingling, reduced sensitivity to one or more structures of the lower limb, burning, electric shocks, strong pricking pain, etc.);
- Reduction in general mobility of the lumbar spine and pelvis, with slowing down of movements in the attempt to return to the upright position after prolonged sitting;
- Contractures and spasms of the lumbar, dorsal, thigh, leg and calf muscles;
- Possible presence of a palpable and visible "step or step" on the lumbar spine;
- Alteration of posture and walking, with possible lateral and/or frontal inclination, determined by perceived pain;
- Increased symptoms upon palpation of the affected area;
- Generalized syndromes of low back pain and lumbosciatica;
- Lumbar depression, generally accompanied by an accentuated lordosis.
3# What are the causes of spondylolisthesis
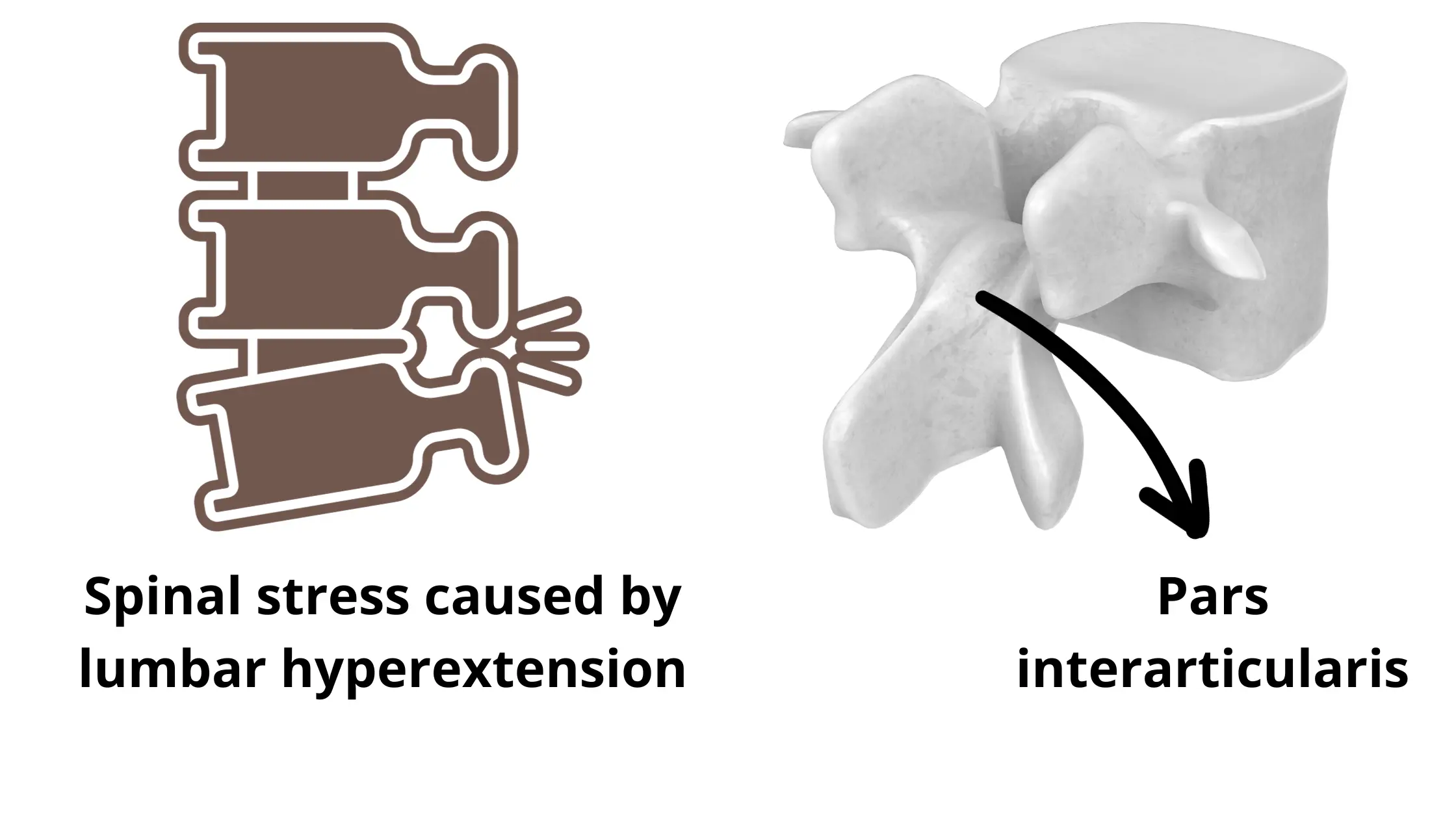
The most common causes are given by:
- Congenital dysplasia:
Some subjects are born with a non-united isthmus (pars interarticularis) and, as time passes, the first symptoms begin to appear, which are refuted by radiographic examination.
- Isthmic injury:
Some physical/sports activities repeated over time lead to an exaggeration of lumbar lordosis, creating excessive stress in the isthmuses of two or more vertebrae.
The consequence is a stress fracture and the vertebra, which no longer has strong support, slips anteriorly.
A spondylolysis is therefore created.
- Degenerative:
The increase in the anterior load by the upper vertebra creates excessive pressure on the underlying one, which in the long term causes premature degeneration of the disc.
Disc degeneration can also occur following instability of the bone segments and joint facets.
It appears most frequently at the level of the L4-L5 vertebrae.

- Traumatic:
Traumas such as falls on the pelvis and road accidents cause micro vertebral lesions, which do not manifest the classic symptoms of spondylolisthesis.
The pain felt at the time of the trauma disappears shortly afterwards and never appears again.
Many professions (such as construction work, removals, etc.) create repeated micro traumas which can lead to the onset of the pathology even years after the initial trauma.
- Pathological:
Pathologies that weaken joint structures (tumors, systemic pathologies, rheumatoid arthritis, infections, etc.).
- Post-surgical:
It may happen that during particular surgical interventions some vertebral structures are removed (this depends on the type of operation and the problem for which the decision to have spinal surgery was made), leading to a compromise in bone stability, which in turn causes the vertebral slipping and the appearance of the classic symptoms of spondylolisthesis.
4# What are the complications of vertebral spondylolisthesis
Complications are represented by the type, degree and angle of bone slip (3):
- Grade 1: 25% spinal slip;
- Grade 2: 25-50%;
- Grade 3: 50-70%;
- Grade 4: 75-100%;
- Grade 5: greater than 100% (spondyloptosis and vertebral dislocation).
Complications of the pathology are:
- Lesion of the outermost layer of the spinal cord (lesion of the dura mater);
- Pseudarthrosis;
- Neurological deficits (alteration/total loss of sensitivity);
- Lesion of peripheral nerve roots.
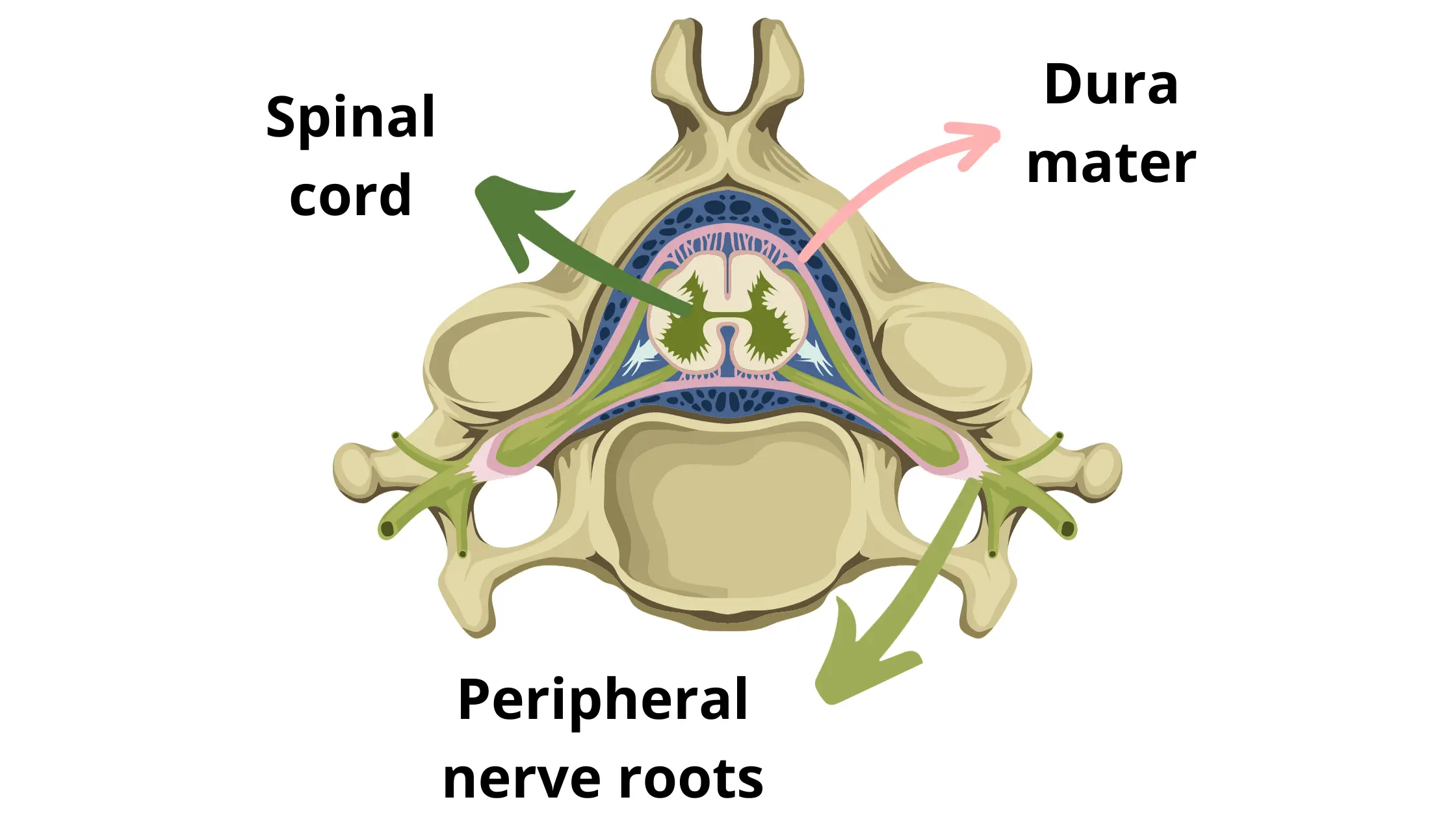
- Cauda equina syndrome (neurological paralysis with diuresis and bowel disorders);
- Failure of the intervention and the means of spinal stabilization;
- Infection;
- Pulmonary embolism;
- Progressive and complete slipping of the vertebra;
- Chronic low back pain;
- Neurological paralysis with diuresis disorders and disability.
5# How the diagnosis of vertebral spondylolisthesis is made
The most suitable instrumental tests for the diagnosis of spondylolysis and spondylolisthesis are:
X-ray:
The lateral radiographic projection allows you to clearly observe the spinal pathology and helps determine the degree and angle of bone slip.
The oblique projection, however, can highlight defects affecting the isthmus and therefore the presence of possible spondylolysis (sign of decapitation of the dog) (4).
Worsening slipping can be assessed by x-rays at six-month intervals, or sooner if symptoms increase.
Magnetic resonance imaging:
MRI provides important information for:
Identify new or old spinal lesions;
Assess the state of the intervertebral discs and any compression on the nerve roots;
Identify a reduction (stenosis) of the spinal canal;
Electromyography:
If neurological symptoms are present, an electromyographic examination can evaluate the impairment and suffering of the central and peripheral nervous structures.
6# What treatments are adopted in spondylolisthesis syndrome and avoid the risk of paralysis
The treatment of spondylolisthesis is defined based on some factors:
- Degree of bone slip;
- Presence or absence of symptoms;
- Fracture of the vertebral isthmus (spondylolysis).
During the visit, the doctor decides whether to start conservative therapy first, or whether to proceed directly to surgery.
Conservative treatment is used in patients presenting with asymptomatic spondylolisthesis syndrome, 1st and 2nd degree.
The most used methods are:
- Rest from any work and sporting activity;
- Non-steroidal anti-inflammatory drugs – NSAIDs;
- Infiltration (cortisonic);
- Physiotherapy and rehabilitation.
Surgical treatment is indicated in the following cases:
- The symptoms progress from an acute to chronic stage (over 3 months) and are disabling/disabling;
- The pain is increasing, compared to the onset of symptoms;
- Conservative treatment did not guarantee the right benefit after 6 months;
- 3rd degree of bone slip.
The surgical intervention aims to:
- Reduce pain;
- Improve the patient's quality of life;
- Correct the deformity;
- Reduce and resolve symptoms;
- If involved, reduce compression on the nerve root.
During the surgical operation, the medical team decompresses the vertebral structure through a procedure called laminectomy (removal of the vertebral plate).
Subsequently, the affected vertebrae are stabilized through arthrodesis and incarceration of the interbody joints.
For the next 30 days, you will be asked to wear a brace to minimize lower back strain.
7# What to do and not to do with spondylolisthesis?
If the symptoms are already present, or you want to try a conservative and therefore preventive approach, your doctor may advise you to change your job and sport, with less physically demanding activities.
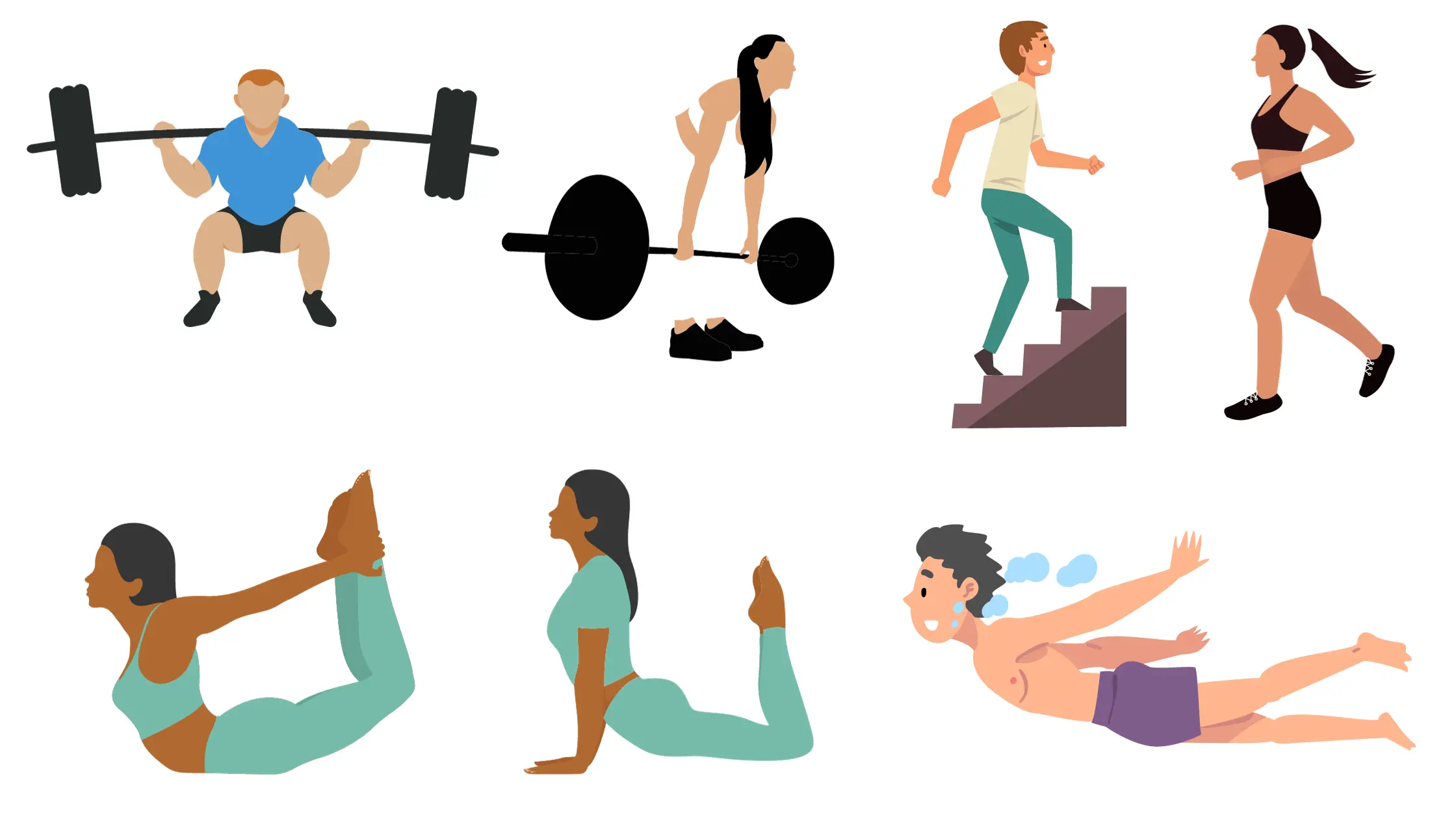
The main activities not to be done to prevent the symptoms from worsening include all those efforts in lumbar and cervical extension.
For example:
- Squats, deadlifts, torso twists, running, uphill walking, breaststroke and freestyle swimming, activities that increase the load on the lumbar spine.
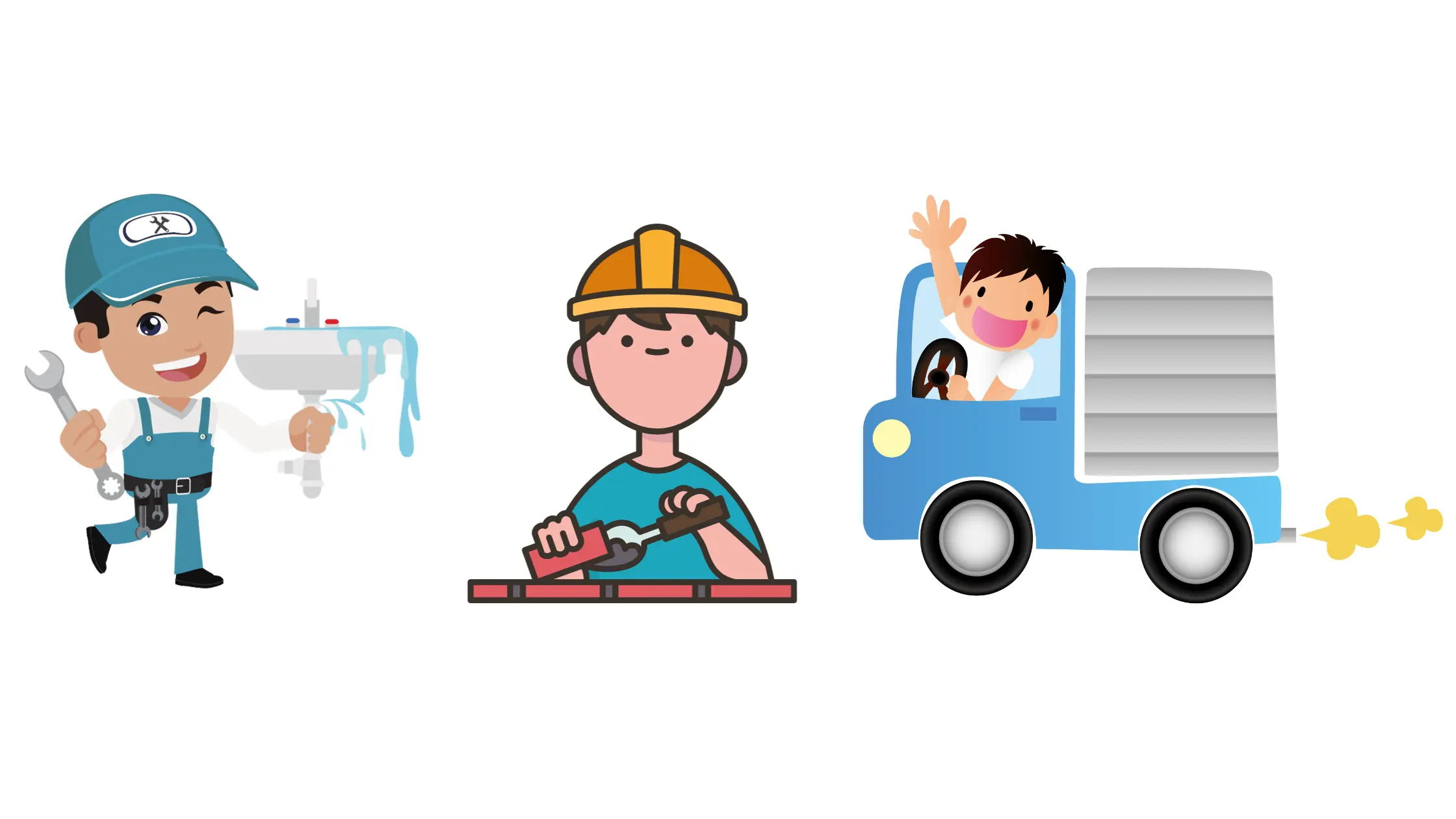
- Jobs as plumber, bricklayer, truck driver, etc.
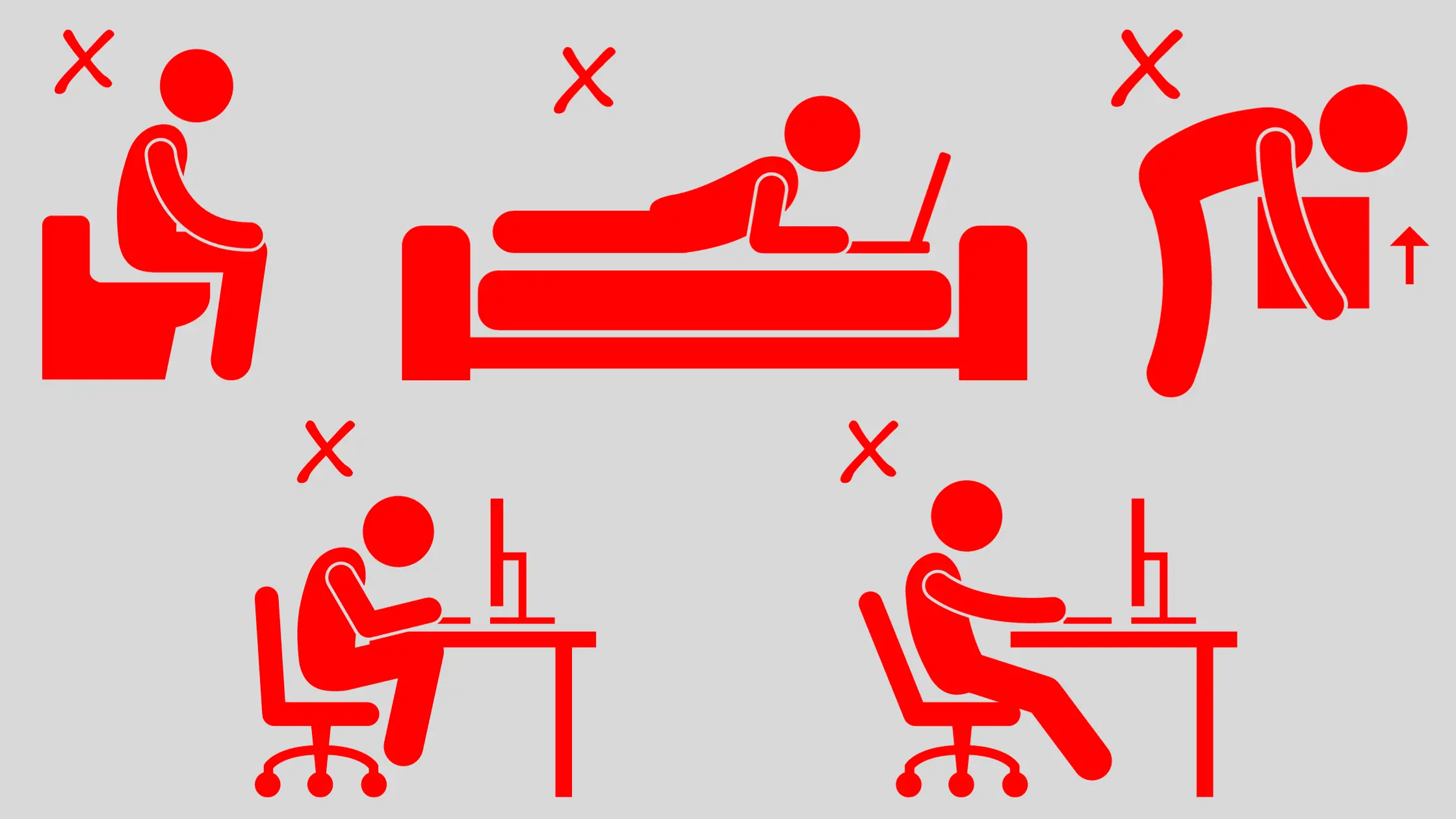
- Incorrect postures at work, at the computer, at home, etc.
The activities that are permitted even in the presence of spondylolisthesis are those that place the greatest strain on the lumbar and cervical spine in flexion.
For example:
- Sports activities such as swimming (backstroke and freestyle), cycling, canoeing, gym (Pilates courses, yoga postures in which the body does not forcibly extend), etc.;

- Sedentary jobs (paying attention to correct posture in the chair);
- Jobs that give the possibility of moving from sitting to standing for a not excessively long time (healthcare worker, doctor, nurses, etc.):

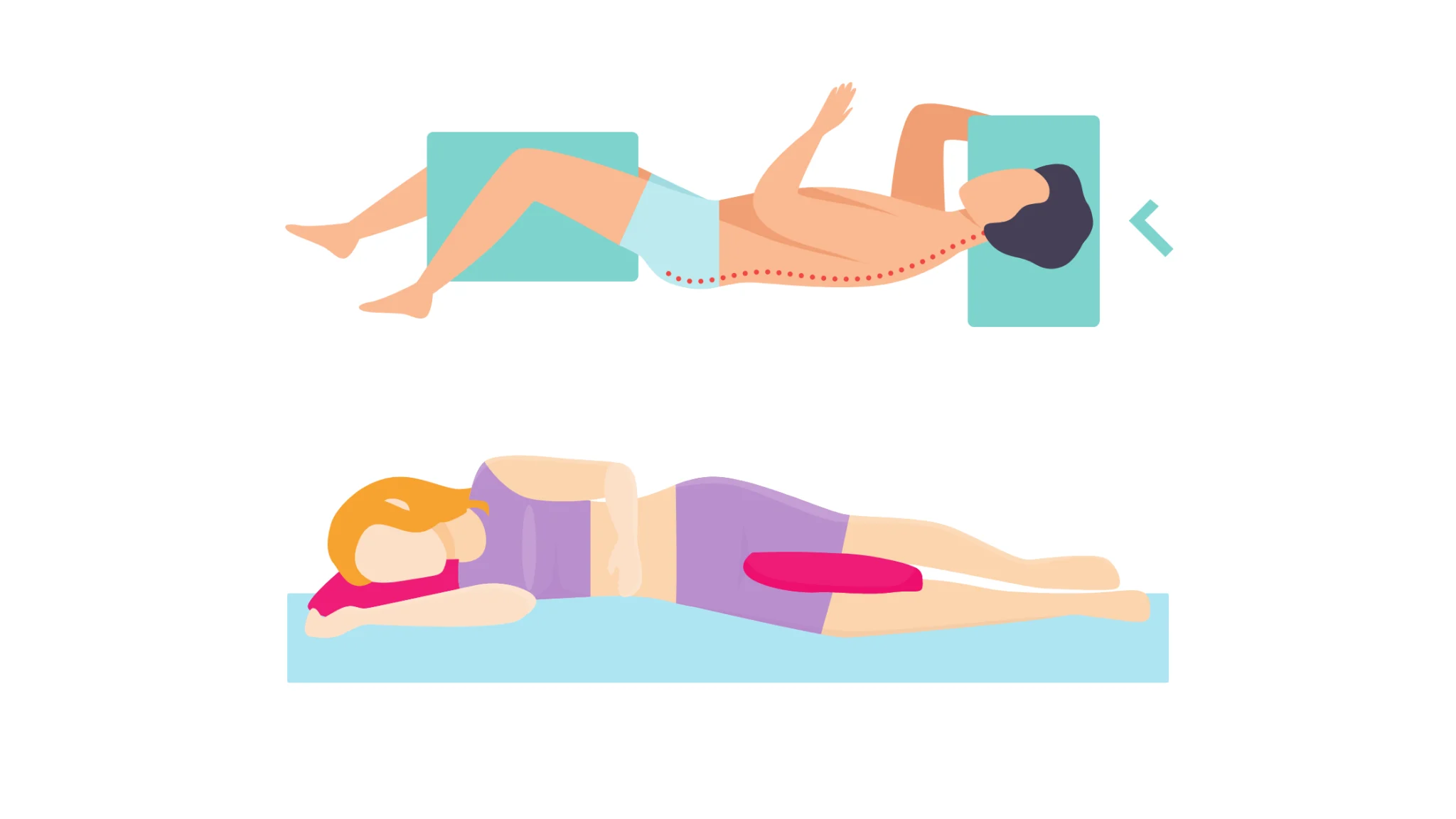
8# How to sleep with spondylolisthesis?
There is no perfect position for sleeping with spondylolisthesis.
This depends on multiple factors, for example:
- Symptoms, degree of vertebra slippage, etc.;
- Type of bed (mattress, sofa bed, etc.);
- Taking medications;
- Presence of spondylolysis.
The best solution is the one that gives you a feeling of greater well-being, without causing an increase in pain.
The positions that you can consider anatomically "the best" are:
1. The fetal position:
The fetal position on one side allows you to obtain greater relaxation of the back and cervical muscles.

It is among the most commonly adopted positions in case of lower back pain caused by hernias, disc protrusions, etc.
Place a pillow between your knees to properly align your spine, pelvis and thighs.
2. The reclining position:
The reclining position for sleeping is not among the most recommended, as if the spondylolisthesis present is of the isthmic type, you may experience an increase in pain and symptoms.
If, however, you feel a sensation of relief and the symptoms do not appear, establish the right degree of inclination based on the well-being felt.
Especially if it allows you to rest adequately.

3. On your stomach, with support under your knees:
Sleep in a supine position (lying on your back, stomach up), could increase the pain.
This is caused by hyperextension of the neck and back.
Then place a pillow or a rolled towel under your knees and under your neck, to allow your back to straighten both curves (i.e. when your neck and back adhere completely to the mattress, without forming an "empty" area).
Even an excessively soft mattress can work in your favor and helps to flatten both the cervical and lumbar lordosis.

4. On your stomach, with a pillow under your belly:
Lying on your stomach can benefit the lumbar spine, but at the same time excessively compress the cervical spine.
The head is rotated laterally and places stress on the neck, shoulders and shoulder blades.
If sleeping on your stomach is the only way to get the right amount of sleep, place a pillow between your pelvis and lower abdomen.
Also use a simple donut pillow (like those also used for massages) or a rolled towel, which covers your forehead and face, giving you the opportunity to breathe correctly and relax all your facial muscles.

5. The military exercise crawl position:
The position allows you to lie on your stomach, avoiding excessively overloading the cervical spine and keeping the lumbar region relaxed.
Lie on your stomach with your head turned to the right.
With your arms at your sides and your palms facing up, bring your right arm overhead until your elbow is bent at 90 degrees and your hand is near your head.
Move your right knee outwards, also bent around 90°.

Bibliography:
(1) J. Maheshwari and Mhaskar. Essential Orthopaedics Including Clinical Methods; Jaypee Brothers Medical Pub; 6°edition (January 1, 2019).
(4) Federico A. Grassi, Ugo E. Pazzaglia, Giorgio Pilato, Giovanni Zatti. Manual of orthopaedics and traumatology; Elsevier; 2° edition (1 Dicembre 2012).